Sexual Health
On this page:
Taking a sexual health history Sexual health testing Downloads
Sexual health is an important part of many trans people’s healthcare. What sexual health looks like for trans people is very similar to that of cis people, but with a few differences. In order to support and affirm your patients, understanding these differences will go a long way to establish a trusting relationship.
Taking a sexual health history
Trans people have all kinds of sex, with all types of bodies. Knowing someone’s gender, their gender history, or even what body parts they have won’t necessarily tell you the types of sex they’re having, or their risk profile.
The only way to know someone’s sexual history, and their level of risk, is to ask them affirming questions that will give you useful answers. In many cases asking these questions is medically necessary and relevant, which makes them even more important.
It can be helpful to let people know you won’t ask things that aren’t necessary to their healthcare. Asking invasive questions without giving a reason why can contribute to a trans patient feeling unwelcome or uncomfortable, and unlikely to return.
Parts and Practices
The parts and practices model focuses on the body parts a person has, and what they’re doing with them, rather than making assumptions based on their gender, sexuality, or the language they use. This model can also be helpful if you’re struggling to find the correct language for people’s identities.
"Do you have sex with people with a penis, people with a vagina, or both?"
"During sex, do any parts of your body enter your partners body, such as their genitals, anus, or mouth?"
"During sex, do any parts of your partner’s body enter your body, such as their genitals, anus, or mouth?"
"Do you or any of your partners use any barriers, such as condoms, gloves, dental dams, or PrEP?"
"Is there a risk of pregnancy for any of the sex that you’re having?"
In some cases it can be helpful to ask about the sexualities or identities, such as in the case of providing STI testing related to priority populations.
"Do you or any of your partners have sex with gay, bi, or queer men?"
"The reason I’m asking about any receptive sex you’re having is so we can figure out what STI tests you might need today."
While it is important to ask for some intimate information, it is equally important to only ask about what you need to know, and to give a reason why you’re asking.
Being clear and honest at the start of the consultation can assist in normalising this process and these questions, and let your patient know that you’re there for their health.
Using affirming language
The language we use always matters, but when talking about body parts that can be a cause of distress or dysphoria for trans people, it’s important we do it in an affirming way.
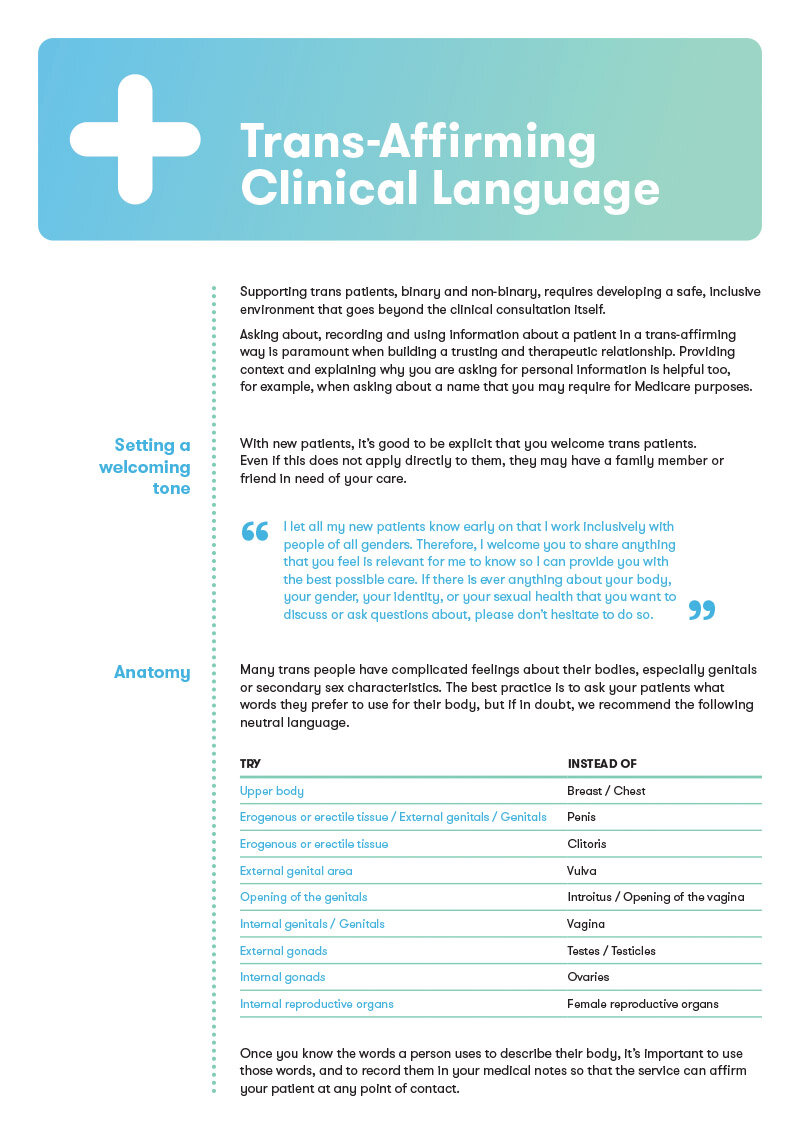
TransHub has put together the resource ‘Trans-affirming Clinical Language’, in which you can read more about how to support your trans patients with the language you use.
The table below from that guide shows some ways you can use neutral language to talk about bodies but still be clear and precise.
| Try | Instead of |
|---|---|
| Upper body | Breast / Chest |
| Erogenous or erectile tissue / External genitals / Genitals | Penis |
| Erogenous or erectile tissue | Clitoris |
| External genital area | Vulva |
| Opening of the genitals | Introitus / Opening of the vagina |
| Internal genitals / Genitals | Vagina |
| External gonads | Testes / Testicles |
| Internal gonads | Ovaries |
| Internal reproductive organs | Female reproductive organs |
Using a patient registration form like this example [PDF] allows you to ask patients about the language they prefer for their body before you even see them, so you can use it from the moment they arrive. If you don’t have these options on your registration paperwork, it’s also okay just to ask.
"Before we get started, I’m going to take a brief sexual history – do you have any language you prefer to use for your body or your genitals so that I can help you feel comfortable?"
If you are ever unsure what a term means, ask your patient to clarify. Trans people may use a range of different words to describe our bodies or sexual practices, eg. a trans woman calling her genitals a vagina, or a person using a colloquial term for a part of their body.
Sexual health testing
Trans people can be tested for all of the same bacterial and viral infections as cis people, and should be assessed for risk and testing needs based on their sexual activity.
An asymptomatic sexual health testing should include screening for chlamydia, gonorrhoea, and syphilis. The testing site will depend on what kinds of sex the patient has been having.
All people with penises should be offered a urine sample. For anyone who has a vagina/front hole, it is also recommended to offer a urine sample, as depending on the type of vagina and the person’s hormonal history, a vaginal/front hole swab may be ineffective or painful. Offering everyone who accesses a service a urine sample is an easy way of not making assumptions about their bodies or genitals.
It is also possible to test for blood borne viruses including HIV, hepatitis B, and hepatitis C. You can refer to the STIPU guidelines here for testing guidelines that include trans men who have sex with other men. For all other trans and gender diverse people, test according to their sexual activity. The Australian STI Management Guidelines for trans people can also be found here.
Human Papilloma Virus (HPV)
Many people with a vagina/front hole are at risk of HPV, and may benefit from the HPV vaccine. People with a cervix, who are within cervical screening guidelines, should be supported to access recommended Cervical Screening Tests (CST), while taking into account that many trans people with a cervix find the cervical screening process uncomfortable or painful.
It’s important to work with your patient to help them understand what is involved in a CST, and the ways they can feel more comfortable and in control. This resource, created by The Inner Circle, includes a list of options that patients can choose from to help them feel more in control of the process. For people who have been on testosterone for some time, a prescription of topical estrogen applied prior to the screening may help them to be more comfortable.
Self-collected CSTs are available under Medicare for patients who meet the following criteria:
over 30 years of age
never had cervical screening, or
are overdue by 2 years or more (ie. 4 or more years since their last Pap test)
Self-collection should not be offered to people who:
are pregnant
have possible symptoms of cervical cancer (bleeding, pain or discharge)
are under the age of 30
have had a hysterectomy and a past history of High Grade Squamous Intraepithelial Lesion of the cervix.
Additional guidelines for self collection of CSTs are available here.
Services like CheckOUT, trans[TEST], and T150 provide affirming cervical screening tests for all trans and gender diverse people, and you can find out more about this at Cervical Screening.
Sexual function
“Do you have any questions about your current sex life, or is there anything are concerned about that I can help you with?”
For some trans people, hormonal and/or surgical affirmation may alter their sexual desires and function. If this is the case, it is important to ask how your patient may want to treat this, if at all eg. For some trans women, the impact of estrogen on sexual function is welcomed, whereas for others, these changes are not wanted at all.
A conversation that asks what changes they’ve experienced, and what changes they feel comfortable or uncomfortable with can open up a space to talk about how you may be able to assist them.
This may look like:
Prescribing topical vaginal/front hole estrogen for insertive sex, and talking about the benefits of lubricant
Supporting a trans person exploring sex for the first time after an affirmative genital surgery
Directing your trans patient to a mental health professional to discuss any difficult feelings they’re having about changing sexuality
Working with a trans patient to alter their hormones or to prescribe medication to better stimulate genital or reproductive function
Reassuring all patients that changing sexual inclination and function over a person’s lifetime is normal, but that you can support them if they want to explore changing what this looks like
PEP and PrEP
HIV Post Exposure Prophylaxis (PEP) and HIV Pre Exposure Prophylaxis (PrEP) are an important and underutilised area of HIV prevention for the trans community.
During the sexual health history it may be identified that a person is at-risk of acquiring HIV. PEP and PrEP are effective methods of preventing HIV, and are safe to use with affirming hormones.
PrEP does not affect a person’s hormones, however, recent research has found that feminising hormones may reduce the efficacy of tenofovir, one of the ingredients of PrEP. It is unclear if this means PrEP is less effective but it does mean PrEP is slightly more complicated for trans people using feminising hormones.
Daily dosing is currently the only recommended PrEP regimen for a trans woman using feminising hormones and trans men who have frontal sex. Non-binary people should consider the right PrEP dosing regimen based on sexual practices and hormone use. This ASHM Decision Making tool also speaks to the guidelines for prescribing PrEP for trans people. For further detail, head to ASHM’s PrEP Guidelines.
Downloads
10 trans questions to ask a doctor - TransHub [ Plaintext version ]
10 tips for clinicians working with trans & gender diverse people - TransHub [ Plaintext version ]
Trans-Affirming Clinical Language - TransHub
Gender affirming intake form for doctors - TransHub